Reginald Tucker-Seeley, the Edward L. Schneider Assistant Professor of Gerontology at the USC Leonard Davis School of Gerontology, spent the past year in Washington, D.C. as a Robert Wood Johnson Foundation Health Policy Fellow. This prestigious program places health professionals in policy-making residencies so they can get hands-on experience working on legislative and regulatory issues. Tucker-Seeley, an expert on health disparities who focuses on the financial well-being of families as they navigate healthcare, served in Senator Dianne Feinstein’s (CA-D) office, where he met with over 150 constituent groups about health-related concerns, worked on legislation aimed at keeping chemicals out of food packaging material, and worked with the U.S. Senate Cancer Coalition to increase racial/ethnic diversity in clinical trial participation. He spoke to us about how his stint in Washington has influenced his teaching and research at USC and why he believes household financial well-being needs to be part a larger part of the national health policy conversation.
What were the most valuable aspects of your experience in D.C.?
Reginald Tucker-Seeley: Having the opportunity to see the policy process happen, to see how funding decisions get made in the US Senate, and to see how hard folks are working to solve big problems was an amazing opportunity. One of the things that was really instructive was to see the policy prioritization process—how an issue goes from an idea to actual legislation. Also, I think many of us in academia really aren’t trained in how to talk to policymakers or in how to situate our program of research within the larger health policy landscape, which is situated within the larger federal policy landscape. The fellowship experience and working in Senator Feinstein’s office with her really talented health policy staff showed me some strategies that worked and some strategies that could be improved.
Will you incorporate anything you learned into your teaching and research?
RTS: I am teaching the undergraduate social policy course in the Leonard Davis School this spring, and I definitely plan to incorporate what I learned about federal policymaking in Washington, D.C. in that course. I’m a big proponent of case-based learning, where students get to practice the skills that they will need in the subject that is being taught. In Senator Feinstein’s office, student interns can work on a project where they go through the process to actually identify a problem, evaluate solutions, and prepare a presentation for a potential policymaker. I plan to use that model in my course. Understanding the many challenges that present in the process from problem identification to solution identification and implementation will be useful for students interested in health and social policy in an aging society, and learning and practicing these skills in the classroom will prepare them for engaging in the policy process at the local, state, and federal levels after they leave my class.
In terms of research, there were several issues related to health disparities that were raised through the many meetings I had with health-related organizations during my fellowship in Washington, D.C. and especially through the many constituent meetings in Senator Feinstein’s office. One of those health issues is end-stage renal disease, or kidney failure. The U.S. spends close to $35 billion on end-stage renal disease care in this country, which is almost as much as the budget for the entire National Institutes of Health. I learned that African Americans are more likely to have end-stage renal disease and progress to end-stage faster than other groups. These disparities-related issues raised my interest in this area, and understanding these issues in the context of aging and household financial well-being is something I’d like to explore further.
Did being in Washington impact any aspects of your current research on the financial well-being of families as they navigate healthcare?
RTS: I’ve often felt like until someone in a decision-making position has a chronic condition where they’ve had to navigate the current healthcare system or has to care for a family member with a chronic condition, many don’t understood the complexity and lack of care coordination involved, the impact on household finances, and the lack of transparency around pricing and cost. As I was immersed in the Washington, D.C. health policy landscape, I was consistently thinking about ways to include in all health policy discussions the impact on household financial well-being as families navigate healthcare and the substantial problem this will become as the U.S. population ages. Families are struggling, and successful solutions to address the many challenges our current healthcare system is facing must ensure that navigating the current system is not financially ruinous for families. The RWJF Health Policy Fellowship was one of the most remarkable experiences of my career. This fellowship gave me an opportunity to see the federal policymaking process from the inside, and I look forward to bringing that invaluable real-world experience to my teaching and research here at USC.
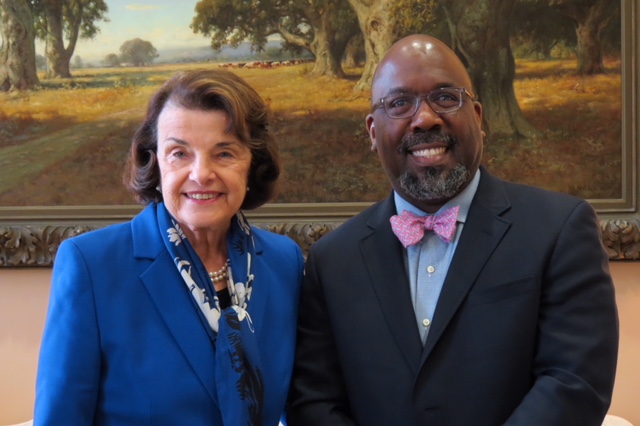
Top: Senator Dianne Feinstein and Assistant Professor Reginald Tucker-Seeley