In an op-ed for TheHill.com, Bank of America Merrill Lynch Global Wealth and Retirement Solutions Head Andy Sieg and USAgainstAlzheimer’s Chairman and Co-Founder George Vradenburg say “social impact investing” can fund innovation and progress in the fight against Alzheimer’s disease.
Read More
The USC Davis School of Gerontology and Marshall School of Business have created a new educational program to provide high-level professionals in senior housing and care the tools to shape the future of the senior living industry.
Read More
USC Davis School of Gerontology Research Professor Henry Forman has earned the Distinguished Service Award from the Society for Free Radical Biology & Medicine.
Read More
More than 50 USC Davis School of Gerontology faculty members and students presented research at the 2014 Gerontological Society of America (GSA) Annual Scientific Meeting held November 5-9 at the Walter E. Washington Convention Center in Washington, D.C. From poster presentations to awards, all facets of the school’s impressive scientific…
Read More

Jim de Vera, student advisor for the Davis School, helps each student make the most of his or her gerontology education. He forges and maintains bonds with students that endure from before the first semester to years after graduation.
Read More
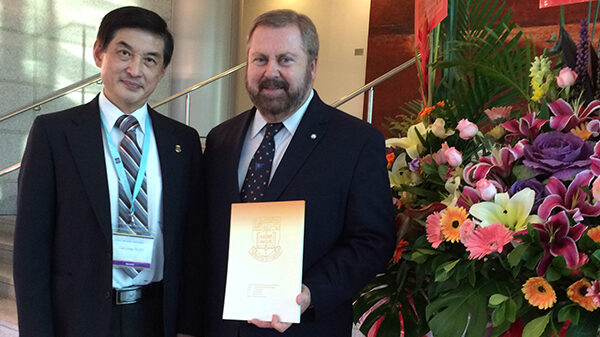
Professor Kelvin Davies, the James E. Birren Chair in Gerontology, Dean of Faculty and Research, and Director of the Andrus Gerontology Center at the USC Davis School of Gerontology, was recently recognized with an honorary doctorate from Guangzhou University and honorary professorships from the University of Hong Kong and Shenzhen…
Read More
As the Baby Boomer population ages, the annual cost of Alzheimer’s disease treatment in the U.S. is expected to nearly quintuple to $1.5 trillion each year, according to a study by Julie Zissimopoulos and Patricia St. Clair of the USC Leonard D. Schaeffer Center for Health Policy and Economics and…
Read More

Just in time for November’s National Entrepreneur Month, entrepreneur Kevin Xu '11 and his wife Leah Yang MASM '13 are announcing a commitment from the Xu family to the USC Davis School of Gerontology to establish the Brighten Award for Entrepreneurial Gerontology.
Read More
The 2014 Caregivers Are Learning More (CALM) Conference and Resource Fair, hosted by the USC Family Caregiver Support Center on November 1, provided valuable education and resources to local community members caring for elderly and/or disabled loved ones.
Read More
USC biogerontologist Valter Longo and Ecuadorian endocrinologist Jaime Guevara-Aguirre are hoping to find the answer in a study of 30 individuals from Ecuador who visited Los Angeles. The researchers hope the results will lead medicine to pharmaceuticals or controlled diets achieving the same apparent protection from major diseases as Laron…
Read More






