










Julie Zissimopoulos is an associate professor in the USC Price School of Public Policy and the co-director of the Aging and Cognition Initiative at the USC Schaeffer Center for Health Policy and Economics, where she’s also a senior fellow and the director of two NIA-funded centers that support innovative social science research on dementia.
She recently spoke to us about her research using economic insights to better understand the impact of Alzheimer’s disease on individuals, families, caregivers, and society.
On the demographics of Alzheimer’s disease
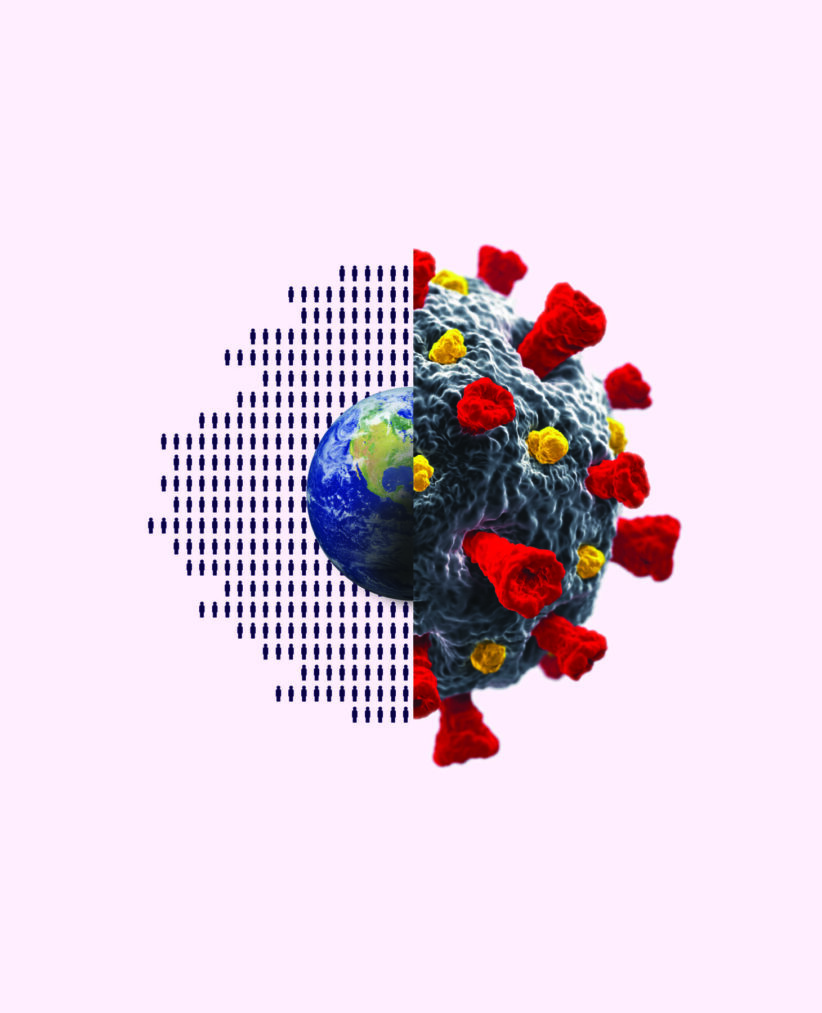
“People are living longer than ever. So, for example, today about 50 million Americans are aged 65 and older. It was about half that in 1950. And by 2050, the US census projects about 20% of the population will be 65 and older. And age is one of the foremost risk factors for Alzheimer’s and other dementias. So what does this mean for our future? Well, it means that without new treatments or innovations or ways to prevent or delay Alzheimer’s and dementia, the number of persons living with this disease will be about 12 million by 2050.
The risk of Alzheimer’s is really a risk at older ages and it rises dramatically with age. So for individuals 65 to 79, about 7% of them will have dementia. But in your eighties, the risk of dementia is about 20% prevalence. And by 85 and older, if you live that long, about 40% of those persons will have Alzheimer’s. It’s also much higher for women than men. And that difference is not explained just by the longer lifespans of women compared to men. It’s also about one and a half to two times higher for Blacks, Hispanics, American Indians, and indigenous Americans compared to whites. And we know a little bit about what explains some of the differences by race. Some of its explained by education and prevalence of chronic conditions that are associated with a higher risk of dementia, like hypertension and diabetes, but it does not explain it all.”
On cognitive assessments at wellness visits
“We collected data from a nationally representative sample of older Americans to understand better their use of annual wellness visits and the cognitive assessments. And what we found that was only about a quarter of them who received an annual visit also reported receiving a cognitive assessment. And this was higher for beneficiaries who were in Medicare Advantage-type plans versus those who were in the traditional Medicare plans. And this might have an important indication that these traditional benefit plans, the Medicare benefit plans, where there’s direct service-related payment for a set of bundled services, like at the annual wellness visit, may not be a very efficient way to increase our cognitive assessments. We also, I think, have some opportunities to improve our policy around cognitive assessments. Right now there’s no guidance about what constitutes a cognitive assessment or how it should be performed. So a clinician can use a structured tool, which we have many of, or they might just ask the beneficiary, the patient if they’re concerned about their memory. And so all of these factors may affect whether we are actually providing good early detection or not.”
On the costs of Alzheimer’s
“Along with the incredible health toll that Alzheimer’s and dementia takes on a person and their families, it also takes an incredible, tremendous financial on the person who’s living with dementia and their family. Alzheimer’s disease leads to cognitive decline slowly destroying brain functioning. It also leads many to behavioral and psychiatric disorders and declines inability to self-care, functional status. And all of this is extremely, extremely costly. So we estimated the costs for all the persons with Alzheimer’s disease, other medical care costs in long-term care costs, and it’s about $200 billion. But that’s only a partial portion of the costs. So as I mentioned persons with dementia need a lot of care and much of this care is provided by family members, unpaid care. And if you value the hours of family members caregiving, that’s about a hundred billion dollars So we’re talking about over $300 billion in costs of care for dementia. And this is more than the cost of cancer and heart disease combined.
There is a growing literature… looking at what are these impacts on the unpaid care provided by family members and other caregivers. And there’s very consistent evidence that there is negative health effects, particularly on mental health. Caregiving for a person with dementia, particularly as the disease progresses from mild symptoms to severe is a very stressful type of caregiving. There’s a very long arm of financial impacts. For spouses, wealth is consumed to pay for long-term care. So care in a facility such as a nursing home can cost anywhere between $50-100 thousand a year. And most families don’t qualify for Medicare that reimburses for the cost of long-term care. And for adult children who are caregivers, there are impacts on their work productivity, their ability to maintain work in the labor force on their income. We don’t have, as a nation, national family leave policies to support and pay for time away from work for caring for older family members with dementia or other conditions.”
On the need for policy changes
“I think one important policy change is we need solutions to support family caregivers in the workplace, compensation programs. But this isn’t going to be enough. Demographic trends suggest that family caregiving as the main source of care is likely not sustainable. People are having fewer children and they are more Americans with dementia. So we really need an insurance system to cover long-term care. The current system does not function well who, who take it up, tend to only be those at high risk with very high healthcare costs. So we need to be a little innovative here, maybe consider a voluntary auto-enrollment in long-term care insurance with an opt-out much like what has worked well in the retirement savings market. Medicare could also help; we had a new benefit of Part D that covers drug expenditures and protects against very high out-of-pocket spending for those beneficiaries with high drug expenditures. This was very successful. Medicare could do something similar for long-term care, but it will be very costly. So we will need to figure out who will pay, how we will finance this and, and, and who is going to bear the costs of this. Will it be the younger generation through taxes on, say, health insurance premiums? If so, how are we going to make sure that they don’t bear the full burden?”
On future research goals
“I’m very interested in continuing to try to understand how drugs for our chronic conditions are affecting our risk of Alzheimer’s. Looking at anti-diabetics right now, and some of those drugs that are potentially increasing the risk of Alzheimer’s and dementia. I’ve been working on understanding and reducing barriers to early detection, how we might improve that and have some real impact there. And then there are many policy changes that are happening to Medicare, new benefits and Medicare advantage and these could all impact the care and quality of life for persons living with dementia. And it’s important for us to understand what care systems best serve the needs of those individuals, protect against financial impacts for them and their families.”
On the importance of social science research
“…Social science has a lot to offer in terms of identifying opportunities to reduce risk, reduce disparities in risk and improve quality of life and care, and really reduce financial burden. And at the USC Schaeffer Center for Health Policy and Economics and in collaboration with the school of gerontology, we have two NIH-funded centers that support grant awards and mentorship opportunities for social science scholars who are interested in this area of research. Through efforts like this and growing this area of research, I think we can make an immediate impact while we hopefully wait for clinical development of that drug that everyone is hoping for.”