Currently, more than 5 million Americans suffer from Alzheimer’s disease, and that number is expected to rise to 16 million by the year 2050, according to the Alzheimer’s Association. It’s now the sixth leading cause of death in the U.S., killing more people each year than breast cancer and prostate cancer combined. Scientists at the USC Leonard Davis School of Gerontology study the memory-robbing illness from several angles in hopes of uncovering the deepest mechanisms of the disease and finding tools for prevention and treatment.
Air pollution a possible cause of a fifth of Alzheimer’s cases
“What’s good for the heart is good for the brain, and vice versa,” says USC University Professor Caleb Finch. He has studied the Tsimane people of Bolivia, a population unusually resistant to both heart disease and dementia, as well as populations here in the U.S. exposed to high levels of air pollution that face higher risks for both cardiovascular disease and Alzheimer’s.
A recent study led by Finch and colleagues found that older women who live in places with fine particulate matter exceeding the U.S. Environmental Protection Agency’s standard are 81 percent more at risk for global cognitive decline and 92 percent more likely to develop dementia, including Alzheimer’s. If their findings hold up in the general population, air pollution could be responsible for about 21 percent of dementia cases, according to the study.
“Microscopic particles generated by fossil fuels get into our body directly through the nose into the brain,” Finch said. “Cells in the brain treat these particles as invaders and react with inflammatory responses, which over the course of time, appear to exacerbate and promote Alzheimer’s disease. Although the link between air pollution and Alzheimer’s disease is a new scientific frontier, we now have evidence that air pollution, like tobacco, is dangerous to the aging brain.”
Animation: Meg Rosenburg
Neighborhood stressors put at-risk people in more danger of Alzheimer’s
Assistant Professor Jennifer Ailshire adds that the relationship between pollution and brain problems in older people is multifaceted. Previous studies have shown that the aging brain is more vulnerable to stress, and the effects of air pollution on cognition appear to be more pronounced in neighborhoods with more stressors, such as crime, disorder and decay. In addition, individuals who had other health problems that impacted the brain, such as stroke, had a higher risk of more pronounced cognitive losses when faced with air pollution than their peers without brain health issues.
Conversely, higher levels of education seem to protect older adults from cognitive losses connected to pollution; even with the same level of pollution exposure, individuals with more education performed dramatically better on brain function tests, Ailshire says. The idea that education can protect against cognitive problems later in life is known as “cognitive reserve” and is an example of how socioeconomic factors can influence health at older ages.
Los Angeles, while having made great strides in managing air pollution in the last few decades, still has some of the nation’s highest amounts of fine particulate matter on average. This adds a new layer to the discussion of helping older adults age in place healthfully, Ailshire says. Even if a home is designed to help residents remain independent as they age, living in a neighborhood with heavy exposure to air pollution could exacerbate health problems and lead to declines in physical and mental function.
Diet and genes interact to influence Alzheimer’s risk
A diet high in cholesterol, fat and sugar may influence the development of Alzheimer’s disease in people who carry the ApoE4 gene, a leading risk factor for the memory-erasing disease, indicates a study led by Professor Christian Pike.
For the study, researchers at the USC Leonard Davis School compared the effects of a poor diet on groups of mice that either had the Alzheimer’s-associated ApoE4 gene or the relatively benign variant of the gene, ApoE3. After eating an unhealthy diet, the mice with the ApoE4 gene showed more Alzheimer’s plaques – a marker for inflammation – in their brains, but those with ApoE3 did not.
“Part of what the results are saying is that risk doesn’t affect everybody the same, and that’s true for most risk factors,” Pike said. “Your genes have a big role in what happens to you, but so does your environment and your modifiable lifestyle factors. How much you exercise becomes important and what you eat becomes important.”
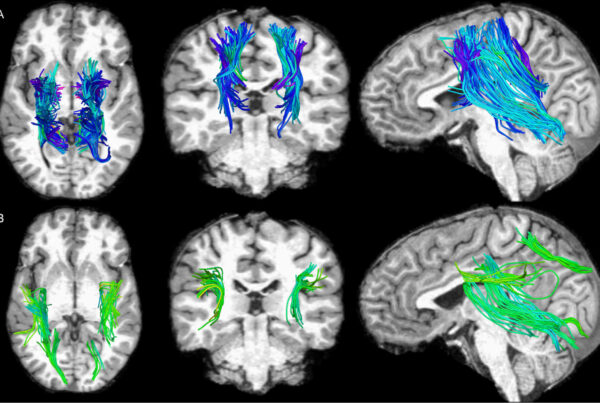
Big data, better imaging technology could stave off brain injury aftereffects, including Alzheimer’s
Following a traumatic brain injury, or TBI, when do the first indications of possible long-term complications—including Alzheimer’s and related dementia—appear, and is it possible to stave them off?
Older adults face particularly high risks from TBI; it’s more common in older adults than any other age group except for infants. A brain injury is also most likely to result in death when it affects a person over the age of 65, with falls being the most common cause for TBI in older adults, says Andrei Irimia, an assistant professor at the USC Leonard Davis School of Gerontology who works to understand the still relatively unpredictable problem.
Irimia has been collaborating with neuroinformatics expert David Kennedy, professor of psychiatry at the University of Massachusetts Medical School, and with Nanshu Lu, an assistant professor of aerospace engineering and engineering mechanics at the University of Texas at Austin. The team’s eventual goal is to give physicians the ability to send mild TBI patients home after an emergency room visit while still monitoring them remotely via easy-to-wear sensors akin to electronic temporary tattoos. The sensors would transmit brain activity data to the computing cloud, which would analyze the patterns and alert the patient and medical team if abnormal brain activity is sensed, Irimia says.
“Right now, we have no way to monitor someone unless they are in a hospital and wired up,” he explains. “If we had a way for clinicians to remotely observe patients after their discharge and spot brain activity abnormalities as soon as they first occur, patients could undergo treatment earlier and the risk for serious problems could be reduced.”